Patient Outcomes
A positive patient experience results in improved financial and patient outcomes. As competition between healthcare providers for patients increases, patients may select their healthcare provider based not only on clinical outcomes, but also on whether their healthcare provider delivers compassionate patient-centered care, in a safe environment.
QPI’s aim is to monitor and report outcomes to healthcare providers and payers that contribute to overall population health.
Quality Measures Management
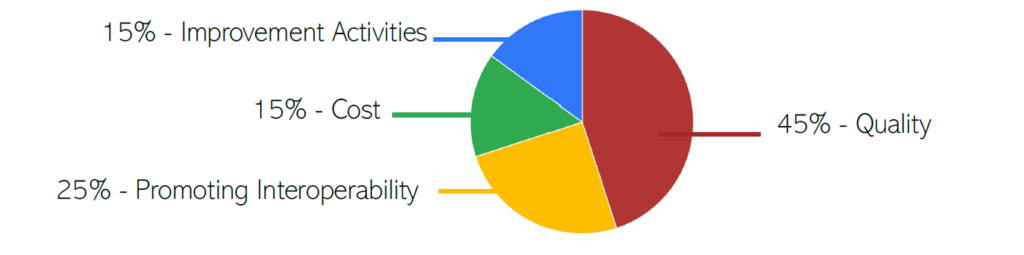
High quality health care is a priority not only demanded by federal, state, and commercial health insurance plans, but also by the US Department of Health and Human Services. Quality initiatives are determined by insurers to assure quality health care for their members (your patients) through accountability and public disclosures. Data collected in 12-month terms, and the weights of their measures, can be submitted to the following pay-for-performance incentive programs:
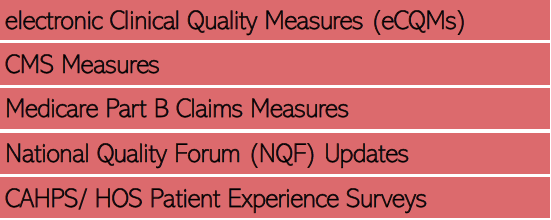
It is QPI’s goal to work with healthcare providers to select measures applicable to your specialty, and begin collecting data for reporting to your organization’s selected pay-for-performance or other mandated program. After all, high quality care is equitable care.
Patient Experience
How do patients perceive their care from their trusted healthcare providers? Should surveys solely rank “satisfaction?” In truly achieving patient-centered care, gauging the patient’s overall experience will allow healthcare providers to further educate their patients on care, treatment or services; focus on addressing dissatisfaction; and showcase positive patient outcomes. Promoting interoperability combines quality data and timely, secure access to care that proves optimization for positive patient outcomes.
Creating a Patient Centric Environment
There is no “I” in “team.” Patient experience is not measured solely by the patient’s experience with the physician, but rather by the patient’s experience with all staff in any healthcare setting.
At QPI, we strongly encourage healthcare providers and their team to seek exemplary patient outcomes by utilizing AIDET.
Patient Experience Surveys
QPI follows the CMS-approved CAHPS (Consumer Assessment of Healthcare Providers & Systems) Surveys. Implementing the leading health insurance plan’s pre-approved survey and achieving positive patient outcomes allows healthcare providers to increase revenue. By providing patient experience reports to pay-for-performance programs, healthcare providers are eligible to receive additional revenue from inside health insurances like Medicare, Medicaid and Commercial Insurance Carriers.
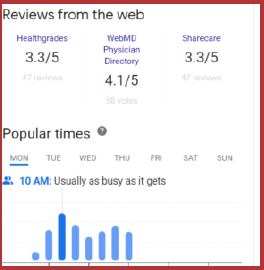
Let’s face it though… word of mouth is the best way to get the message out there. Patients have the option to post their experience on Health Grades, Google and more. QPI will monitor findings to these sources.
CAHPS (Consumer Assessment of Healthcare Providers and Systems)
QPI will conduct surveys for you as an unbiased third-party. Raw data is collected, communicated and analyzed with you, and distributed to pay-for-performance programs and requesting payor sources. Ultimately, aggregated data will be added to Physician Compare or Home Health Compare, available to Medicare patients.
Create and Maintain a Culture of Safety
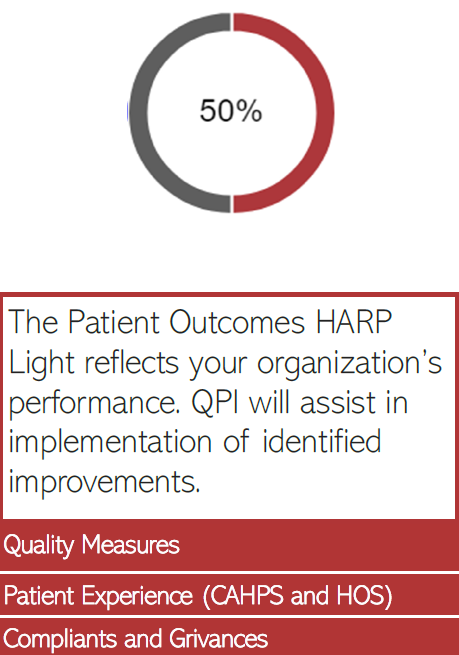
Promotion of patient safety culture can best be conceptualized as a complex series of interventions rooted in principles of leadership, teamwork and behavior change. Strategies to promote a culture of patient safety may include a single intervention or several interventions combined into a multi-faceted approach or series. Several studies show that safety culture and the related concept of safety climate are related to such clinician behaviors as error reporting, reduction in adverse events and in reducing mortality. Safety cultures also protect patient health information. Utilizing HARP Light Technology and our team of well-versed professionals will guide your organization towards interventions that promote a culture of safety.
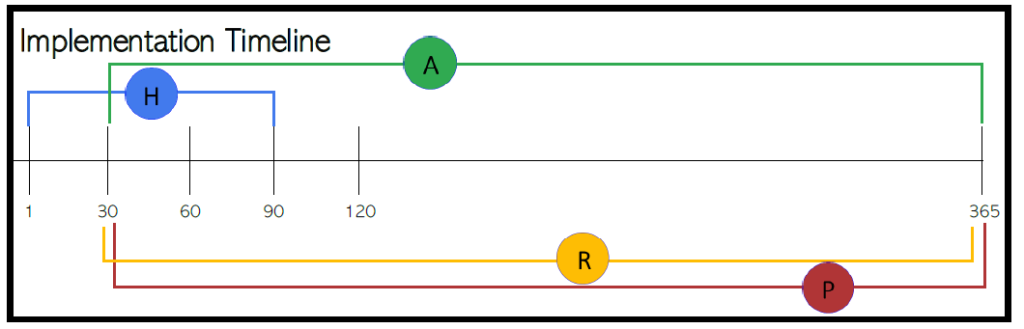
Get Back to What’s Important: Patient-Centered Care
What can QPI Healthcare Services™ do for your organization? Many healthcare providers didn’t become healthcare providers to do paperwork. Truly invested healthcare providers attended school for many years to one day help people and serve their community. Let QPI do the rest. Lavear and HARP Light Technology absorbs a multitude of administrative responsibilities by managing the daily, weekly, monthly, quarterly and annual tasks for your organization. Our checks and balances are strongly aligned with the Centers Medicare and Medicaid Services, The Department of Justice, Office of the Inspector General, State and Local Agencies, Accreditation Organizations and you, our trusted healthcare provider!







