Risk Management
The Importance of Risk Assessments & Management Planning
Given that organizations face unique challenges, there is not a one-model-fits-all risk management solution. Data sets vary from provider to provider as does the collected data from each set. Our program includes providing sophisticated and automated push-technology to our clients as means to specify data sets to collect and analyze measurable performance improvement data, including that of risk management activities.
QPI’s HARP Light Technology is designed to identify your organization’s potential risk, similar to a SWOT Analysis, routinely. Our Risk Management team will effectively communicate with your organization’s leadership team regarding issues that are monitored and evaluated regularly and will establish a risk assessment plan, PDCA, CAP or RCA, as applicable.

Risk Manager Responsibilities (at-a-glance)
Payor Requests
- Appeals & Denials
- Palmetto GBA—SACU Audits
- Development Requests
- Corrective Action Plans
- Commercial Payor Audits
- Site Visit Reports
Regulatory Training
Access to QPI's Legal Counsel
- Fraud, Waste and Abuse Certification
- Anti-Kickback
- STARK
- Communication Hotlines
- Compliance Reviews and Assessments
- Internal Compliance Audits
- Cybersecurity
- Monitor State/ Federal Regulations
Reporting Tools
- Sentinel Events Assessment
- Fire Drill
- Safety Assessment
- OSHA Assessment
- Hazard Assessment
- Incident Reporting
- Annual Evaluation and Review to BOD
- HIPAA Assessment
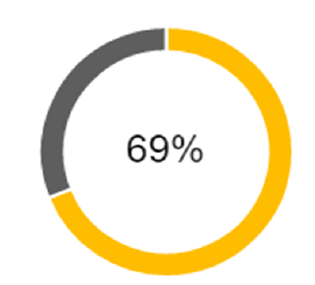
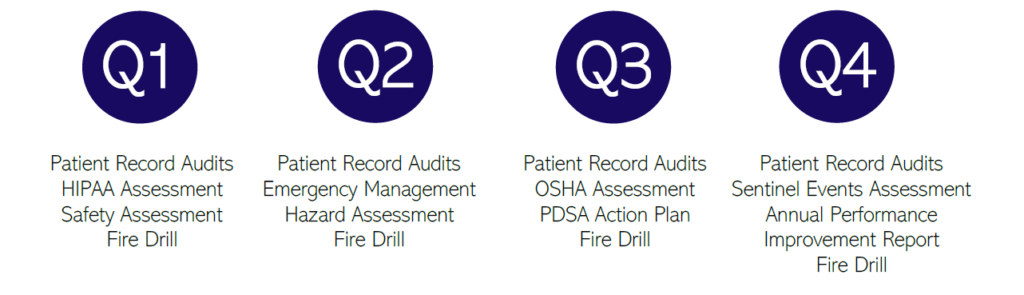
Our Risk Management team is dedicated to facilitating assessments and reports virtually on a quarterly basis.
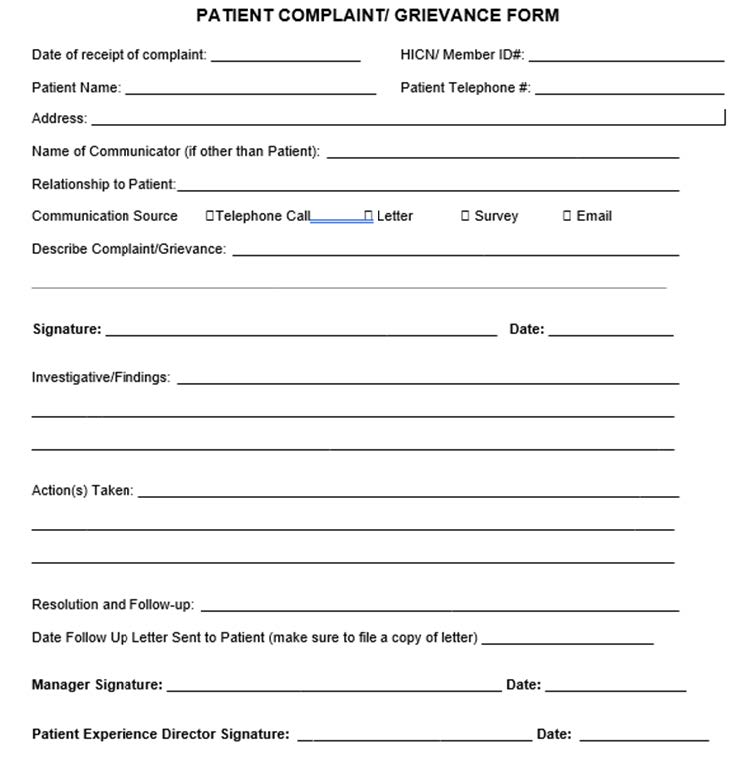
Complaint and Grievance Reporting
Malpractice and NPDB Reporting
One of the largest risks that healthcare providers face is medical malpractice. Negligent acts or omissions that result in patient injury often prompt legal action.
While we work hard to collectively combat this from happening, we understand that these occurrences take top priority. QPI will work diligently with your organization’s leadership team and legal team to ensure appropriate responses and reporting have been completed and submitted.
Upon identifying any incident, including medical malpractice, QPI’s Risk Management Team will notify the National Practitioners’ Data Bank (NPDB) and assist in submitting applicable reports.
National Practitioner Data Bank Reportable Occurrences
- Medical malpractice payments
- Federal and state licensure and certification actions
- Adverse clinical privileges actions
- Adverse professional society membership actions
- Negative actions or findings by private accreditation organizations and peer review organizations
- Health care-related criminal convictions and civil judgements
- Exclusions from participation in federal or state health care programs (including Medicare and Medicaid)
- Other adjudicated actions or decisions
Annual Performance Improvement Report
Managing risks can be daunting. While large risks can occupy the majority of our time, often the smaller, recurring risks are forgotten. QPI’s series of Risk Management Activities collect federal, state, and commercial health insurance plans’ required performance measures such as Medical/ Patient Record Audits, Billing and Coding Error Logs, Patient Complaints, Adverse Events, and more on a weekly, monthly, quarterly and annual basis.
Data collected from Risk Management Activities are analyzed by QPI and reported back to you in an Annual Performance Improvement Report. This report provides a systematic process to monitor all service aspects of health care, as delivered to the patient by your organization. It includes an organized framework to identify opportunities to improve quality and patient outcomes.

For transparency, QPI compiles all performance measures found throughout HARP, year round, for a years’ end Annual Performance Improvement Report. QPI contacts your organization’s leadership team to review and approve all findings in this report, to discuss and identify methods for performance improvement as it applies to federal regulations, state statutes, accreditation standards, local laws and other regulations sanctioned by federal, state, and commercial health insurance plans.
The hazards of not preparing for potential issues can have significant, long-term effects. Neglecting to have comprehensive risk management plans in place can compromise patient care, increase liability risks, and result in financial losses.
Licensing, Privileging, Enrollment & Credentialing
Licensing is a formal process that utilizes an established series of guidelines to ensure that patients receive the highest level of care from healthcare professionals who have undergone the most stringent scrutiny regarding their ability to practice medicine. This assures the patient that he or she is being treated by providers whose qualifications, training, licensure, and ability to practice medicine are acceptable. QPI works with providers and organizations to maintain state and federal licensure renewals. Additionally, QPI works with providers to obtain and maintain privileges/ affiliations with local hospitals, etc. Credentialing ensures that all healthcare workers are held to the same standard. QPI monitors, obtains, and maintains all credentials for accuracy and continued care for uninterrupted patient care.
Credentialing for Licensed Individuals & Organizations
- CAQH—Provider ID—Application/ Attestation
- List of all previous and current practices
- IDs (UPIN, PTAN, Medicaid, NPI)
- Curriculum Vitae
- State Board Medical License
- Health Insurance Plan Requirements
- Telemedicine Credentialing
- DEA Certificate
- CDS Certificate
- IRS Form: W9
- Malpractice Face Sheet
- Summary of pending/ settled malpractice cases
- NPDB Reporting
- Lab Enrollment Services (CLIA)







